Olfactory meningioma
Last edit by Alaric Steinmetz on
Synonyms: Olfactory groove meningioma, OGM
ICD-11: 2A02.1Y
Olfactory meningiomas are meningiomas, which arise from the dura or the arachnoid of the olfactory groove and can present as WHO Grade 1-3 tumors depending on the histological type.
Epidemiology
Olfactory meningiomas are rare and, together with planum sphenoidale meningiomas, account for about 2% of all primary intracranial tumors[^1]. Olfactory meningiomas appear slightly more frequently in women than in men, with a ratio of approximately 1.45:1[^9].
Symptoms
Olfactory meningiomas often remain asymptomatic for a relatively long time and are then often diagnosed at a considerable size. Unilateral or bilateral loss of the sense of smell is usually one of the first symptoms, which is often not recognized by the patients. Most patients present with headaches, visual impairments, or cognitive changes upon initial diagnosis[^9].
Vascular Supply
Olfactory meningiomas frequently receive their vascular supply via the anterior ethmoidal artery and the posterior ethmoidal artery as well as the anterior branches of the middle meningeal artery and meningeal branches of the ophthalmic artery[^2]. In larger olfactory meningiomas, the vascular supply can also originate from direct branches of the anterior cerebral artery or anterior communicating artery [^2].
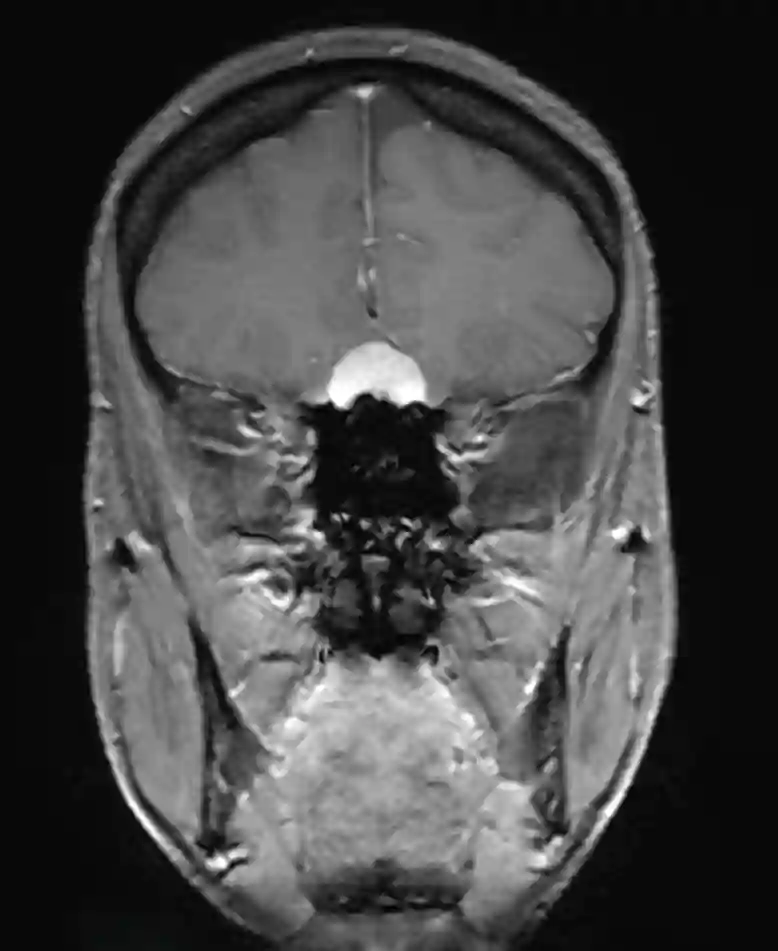
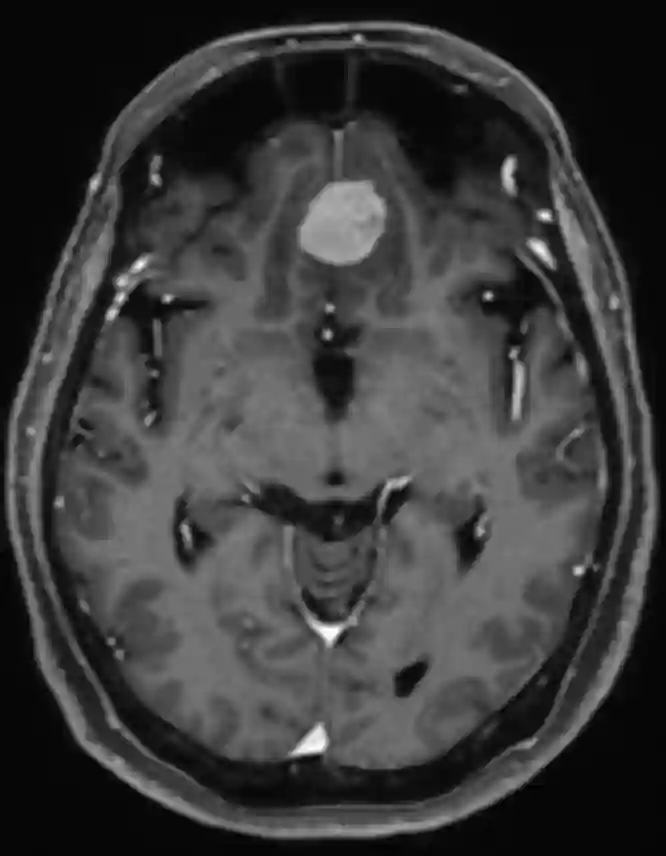
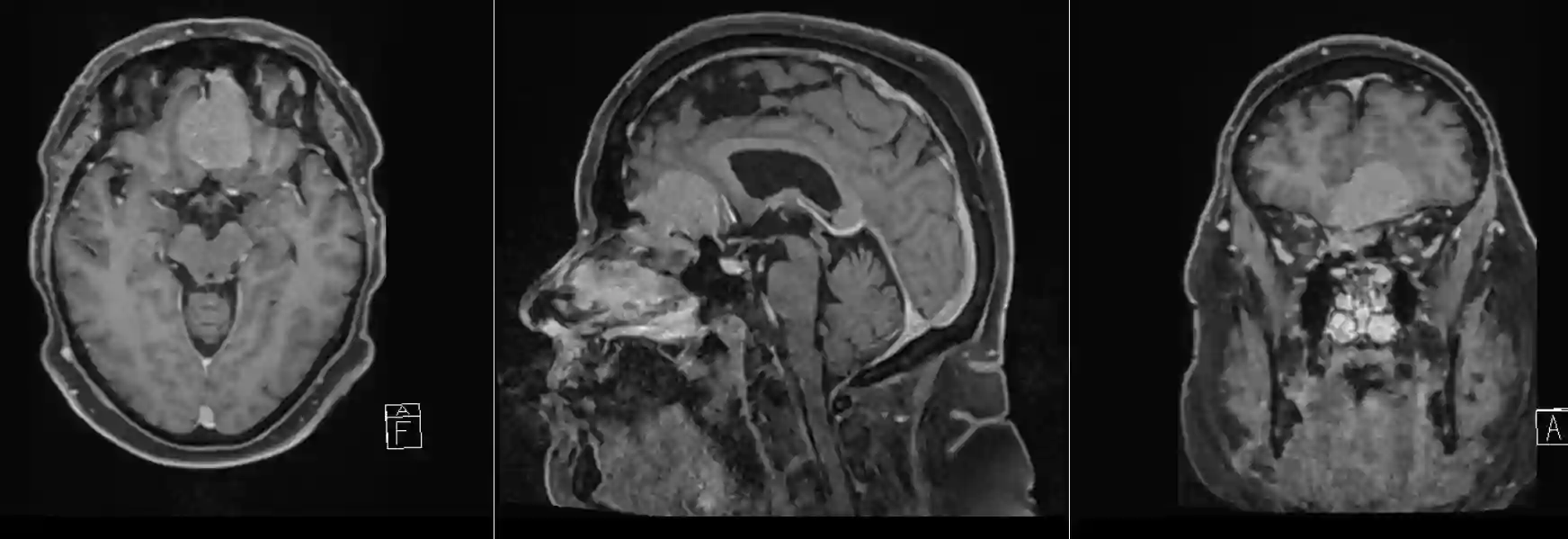
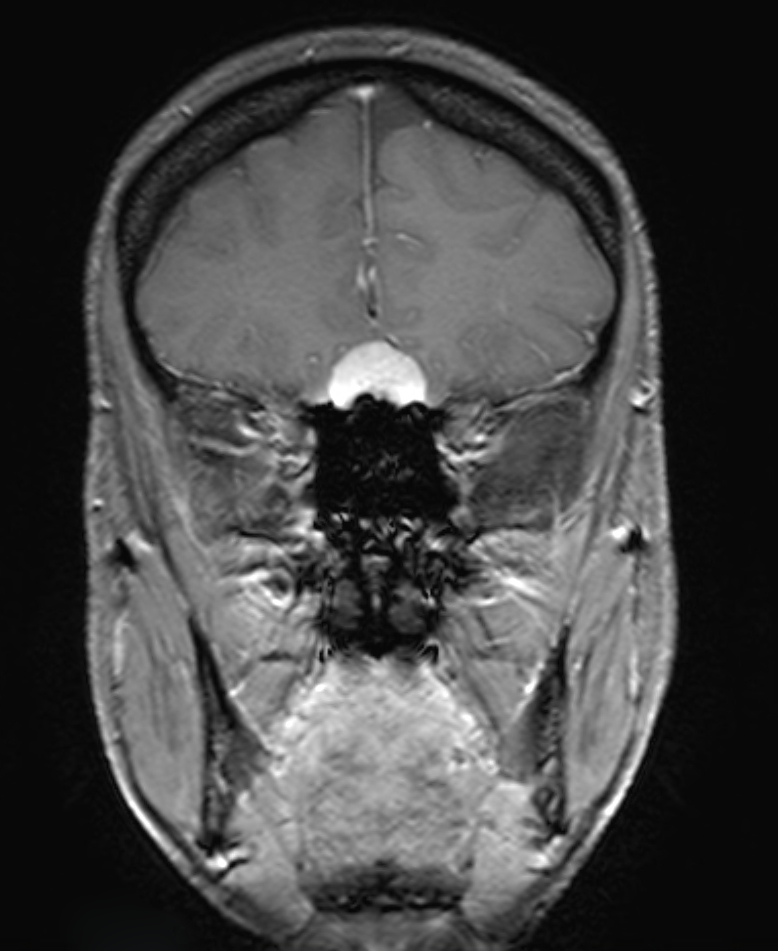
Imaging
The gold standard for imaging of olfactory meningiomas is MRI imaging. A digital subtraction angiography is usually not necessary for preoperative planning, as the vascular relationships of the tumor can mostly be adequately represented in conventional MR imaging[^3].


Surgical Approach
Olfactory meningiomas can be accessed and resected via various surgical approaches.
Subfrontal Approach
The subfrontal approach offers the advantage of early devascularization of the tumor at the skull base. Furthermore, this approach allows for the removal of vascularized pericranium for reconstruction of the skull base. A disadvantage of this approach is the opening of the frontal sinus and the associated increased risk of cerebrospinal fluid fistula and infection. Also, in this approach, the anterior part of the superior sagittal sinus is transected[^3].
Pterional Approach
Through a pterional craniotomy, olfactory meningiomas can also be accessed. The advantage of this approach is early visualization of the optic nerve and the internal carotid artery before tumor manipulation. Additionally, the basal cisterns are reached early in the surgical course so that cerebrospinal fluid can be drained for a better operative overview. A disadvantage of this approach is the limited angle of access to the superior tumor portion, which often requires retraction of the frontal lobe. Moreover, reconstruction of the skull base via this approach is challenging[^3] [^4].
Supraorbital Keyhole Approach
Another option is a supraorbital approach via a keyhole. A study showed shorter hospitalization duration and less postoperative edema in patients compared to the conventional approaches[^7].
Interhemispheric Approach
The advantage of an interhemispheric approach is direct exposure of the tumor with minimal brain retraction and without opening the frontal sinus[^8]. The disadvantage of this approach is the difficult access to the vascular supply of the olfactory meningioma. The surgical corridor is also long and narrow, which can lead to frontal lobe contusions. Depending on individual anatomy, bridging veins may complicate this approach[^3].
Endoscopic Endonasal Approach
The endoscopic endonasal approach has the advantage of direct access to the tumor with minimal brain retraction and the possibility of early devascularization of the tumor[^5]. However, this approach has a steep learning curve and, depending on tumor spread, may not make all intracranial tumor portions accessible[^3] [^6].